General Delta virology:
Researchers have so far identified more than 20 mutations in the delta variant. Two of the 20 mutations are more effective in transmission; This is called a “double mutant.” A new delta strain of SARS-COV-2 belonging to B.1617 (ineage) has recently increased COVID-19 in India. This new delta is divided into three categories in India:
B.1.617.1
B.1.617.2
B.1.617.3
Spike protein type B.1.617.2 contains 9 mutations in the S₁ subunit and one mutation in the S₂ subunit. Also in the S₁ subunit, there are five mutations in the N-terminal domain-containing binding sites for antibody neutralization. There are two mutations in the receptor-binding domain (RBD) of the S₁ subunit that affect antibody neutralization and the extent of contamination of others. Three mutations remain, the other two mutations increasing the binding of the angiotensin-converting enzyme, viral replication, and cleavage of the spike protein at the S₂ S₁ / site.
A good feature of the delta strain is that it is quickly traced and the S mark is used as the “target gene”.

Latency period
The latency period of the delta Variant is very short and after studies, it has been determined that the incubation period of the delta Variant is 4 days. Also, the delta Variant multiplies so fast that within 6 days of the virus, 1260 times more people are infected with the Wuhan (classic) virus.
According to research in the United States, people who have been vaccinated twice as much as those who have not been vaccinated are more likely to get delta Variant diseases. Some people who received two doses of the vaccine but became infected with delta had no symptoms and were only carriers; But in others who had been vaccinated with two doses, they showed signs of COVID-19 after contracting delta.
Therefore, people who have been vaccinated both times but have COVID-19 symptoms should be tested and quarantined.
The AstraZeneca or Pfizer vaccine is 60% and 80% effective against the symptomatic disease, respectively. There is also other evidence that the Johnson& Johnson vaccine is effective against the delta variant. Other research has shown that a single dose of mRNA vaccine or previous infection with CoVID-19 rarely blocks the delta variant.
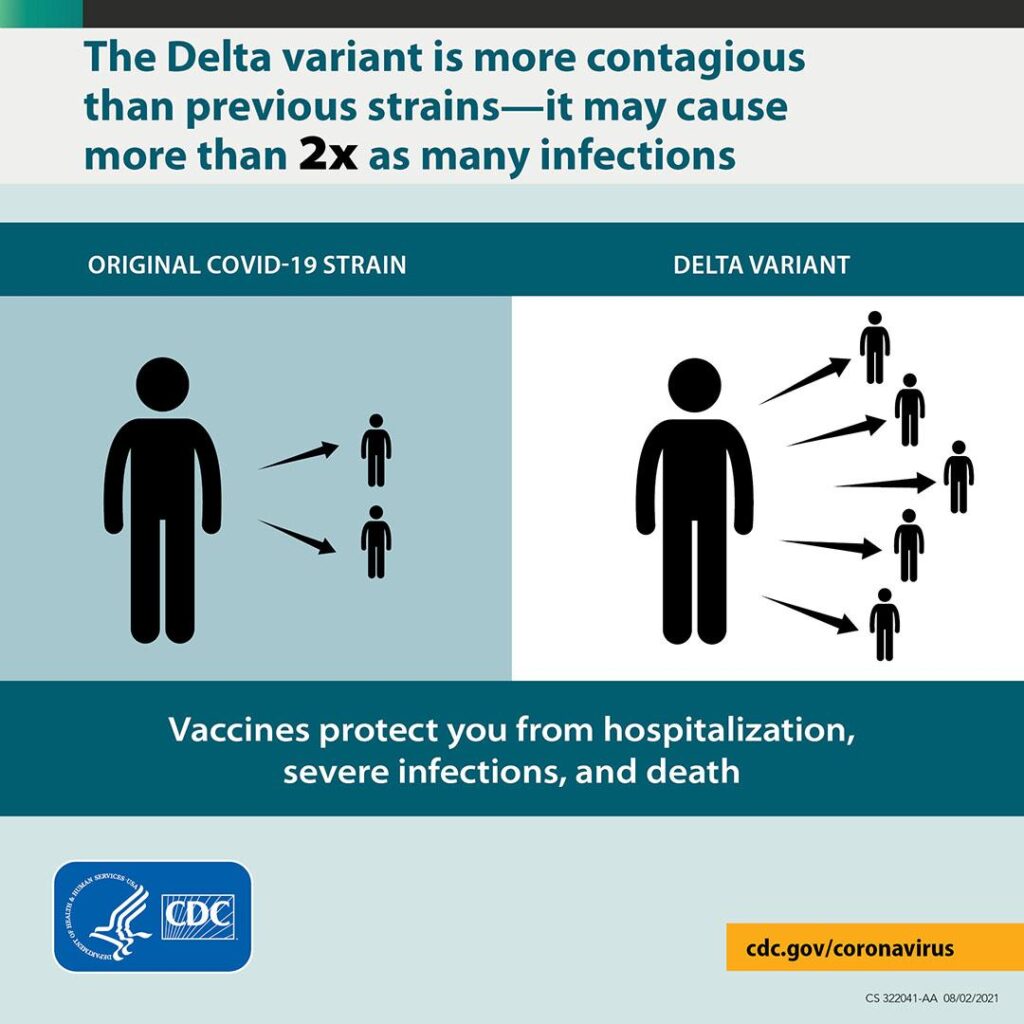
Transmission
Research has shown that the delta variant is 60% more contagious than the alpha variant, and people with the previous coronavirus variants infected two others. People with delta can infect 5 more people.
The lower the rate of vaccination in the community and geographical location, the stronger the delta strain will be in shaping a larger epidemic and pathogenicity. However, if the vaccination rate is high in a community or geographical area and different groups have been vaccinated, then the delta variant will be able to cross from one low-coverage area to another low-coverage area, and an epidemic will develop. This phenomenon is misleading in areas where vaccination rates are very low.
In communities such as rural areas, suburbs, poor countries where there are no sanitation facilities and vaccines, or vaccination rates are very low, the delta variant will be vulnerable to people in that community. In North America, for example, vaccination rates are high, but in South America, vaccination rates are very slow, while people in the South American community suffer from diseases such as diabetes and obesity.
“The delta variant is a special and very dangerous threat to poor countries that do not have access to vaccines, Such as Africa.” said a senior adviser to the World Health Organization.
Immune escape phenomenon
The well-known mechanisms of immune escape that were active in the corona are now acting more strongly in the delta. In CoVID-19, antigen delivery was reduced through MHC classes one and two, but the production of “syncytium” in the SARS-CoV-2 strain occurs more intensely.
The delta variant is more volatile than the made-up antibodies than the alpha or B.1.1.7 variant. This is very dangerous in the elderly due to their low physical strength and less effectiveness than vaccines.
The delta variant travels from cell to cell and reproduces easily without producing antibody risk, producing “senescence“. As a result, it is very dangerous for people who have not been vaccinated because of its escape from the immune system and cell-to-cell proliferation.
Research has shown that one dose of the vaccine: 31% is effective in preventing delta-type disease; It also prevents 75% of hospitalizations.
According to the latest announcements of the country’s health officials and international sources, the only way to deal with SARS-CoV-2 variants at the moment is as follows:
- Increase the speed of vaccination;
- Adherence to health protocols;
- Use of masks;
- Social and physical distance.
Studies show that children and adults under the age of 50 are 2.5 times more likely to get delta variant.
Decreased susceptibility to monoclonal antibodies:
Examination of delta variant for susceptibility to antibodies in the sera of COVID-19 recovering or vaccine recipients were found to be resistant to these antibodies. Serum collections from recovering patients showed that antibody resistance in serum antibodies was four times lower than in alpha patients up to 12 months after delta-based symptoms. Also, the sera of people who received the Pfizer or AstraZeneca vaccine could not control the delta type.
Receiving two doses of the vaccine has produced a neutralizing response in 95% of people. Thus, the increase in delta type may be accompanied by the escape of antibodies targeting non-RBD and RBD spike epitopes.
Scientists tested the effect of four therapeutic monoclonal antibodies in neutralizing B.1.617.2. Bamlanivimab alone could not neutralize B.1.617.2; As a result, Bamlanivimab monotherapy may not be effective in treating B.1.617.2 infection. The other three antibodies showed similar effects in neutralizing both wild-type and B.1.617.2 viruses. Also, antibodies derived from patients with COVID-19 improved, and those vaccinated with BNT162b2 had a lesser effect on neutralizing B.1.617.2 than wild-type virus. Hence type B.1.315 showed a higher ability to escape disease-induced immunity after vaccination.
Increased entry of delta variant into body cells:
The entry of the delta mutant virus into the host cell by means of the spike protein may vary between cell types, and B.1.617.2 has higher pathogenicity in the process of entering the cells of the lung and colon. Because the Spike protein variant B.1.617.2 does not show an increase in ACE2 binding, scientists have hypothesized that an increase in B.1.617.2 entry into colon and lung cells does not occur with an increase in ACE2 binding. Overall, the P681R mutation in the Spike Delta variant protein facilitates cleavage of the protein and enhances viral fusogenicity.
More pathogenicity of delta means that unvaccinated people who become infected with this strain will become sicker and more disabled than before, and therefore need more care.
references:
- https://www.nature.com/articles/d41586-021-01986-w
- https://www.medscape.com/viewarticle/955701
- https://www.medscape.com/viewarticle/955744#vp_3
- https://www.cdc.gov/coronavirus/2019-ncov/variants/delta-variant.html
- https://www.yalemedicine.org/news/5-things-to-know-delta-variant-covid
- https://spiral.imperial.ac.uk/handle/10044/1/89629
- https://www.yalemedicine.org/news/5-things-to-know-delta-variant-covid
- https://health.ucdavis.edu/coronavirus/covid-19-information/delta-variant.html
- https://science.sciencemag.org/content/372/6549/1375
Originally written on: https://payvandlab.com/delta-covid-19-variant-more-infectious/?lang=en


